Intravesical BCG
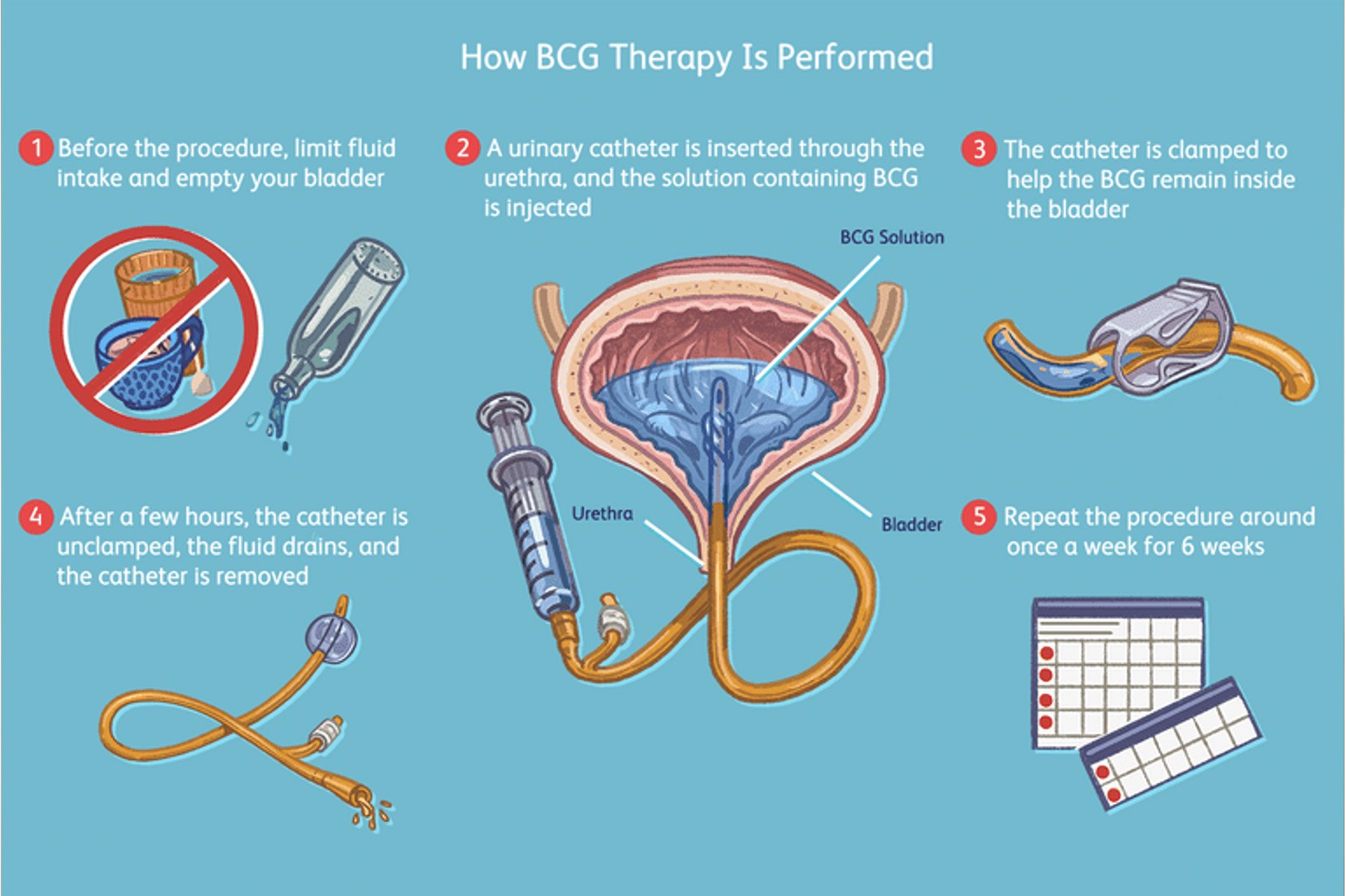
Figure 1: Intravesical BCG instillation
What are the indications for an intravesical instillation?
Instillation of an immunotherapy drug into the bladder is used in patients with aggressive or frequently recurring cancer of the bladder that has not invaded the muscle of the bladder.
The most commonly used drug is BCG although other drugs such as Mitomycin, Epirubicin and Gemcytabine can also be used.
The aim of the procedure is to reduce the chance of the bladder cancer invading the muscle (which then requires more extensive surgery such as radical cystectomy or radiotherapy).
What pre-operative work up is needed?
Your urologist will organise any necessary urine and blood tests and imaging scans at your consultation prior to your procedure. You generally can continue taking your usual medications prior to and after your procedure unless directed by your urologist. If there is presence of infection in the urine, your urologist will organise for you to take some antibiotics prior to your procedure.
You should limit your fluid intake 6 hours before each treatment and take a Ural sachet (urinary alkaliniser, which can be obtained from most pharmacies) dissolved in water the evening before and the morning of your instillation.
Please ensure you return any admission forms given to you to be filled out back to the hospital.
What happens on the day of the procedure?
You generally do not need to fast for this procedure. You should bring a list of your medications, any recent scans or reports with you to the hospital. An anaesthetic is not required for this procedure. A nurse will see you in the procedures ward and explain the procedure to you again.
You should allow 90-120 minutes for the whole process on the day.
On arrival to hospital, we will ask you to pass urine and we will test it for infection. If testing suggests an infection, we will send a sample to the laboratory and may postpone your BCG treatment whilst you take a course of antibiotics.
To deliver the chemotherapy agent into the bladder, a catheter tube is inserted through your urethra (waterpipe) into your bladder (pictured below).
Your genital area will be cleaned with an antiseptic solution and an antiseptic gel containing local anaesthetic will be instilled into your urethra. A small catheter is passed into your bladder and the chemotherapy drug instilled over 5-10 minutes. The catheter will be removed from your bladder and you will be asked to try not to pass urine for the next two hours, to allow the medication to treat the whole bladder lining.
Are there any risks or side-effects of intravesical chemotherapy / BCG?
Urine Infection (10-20%)
Some bladder discomfort (10-20%)
Flu-like symptoms, which can last for two to three days (10-20%)
Urinary frequency and urgency (20-30%)
Blood / debris in your urine (10-20%)
Stricture (narrowing) of the urethra (waterpipe) 5%
Inflammation that can affect various parts of the body 5%
Failure to complete the course due to side-effects 10-20%
Persistent or severe pain after treatment – rare
Generalised serious infection with BCG bacteria - rare
What can I expect when I get home?
For 6 hours after the treatment, you should urinate while sitting to minimise the risk of splashing urine, which contains live bacteria
Pour undiluted household bleach into your toilet after passing urine, and leave this for 15 minutes before flushing the toilet.
You should drink plenty of fluids for the first few days after the treatment
It is best not to have sex for at least 24 hours after each treatment because this can be uncomfortable and for one week afterwards, you should use a condom during sex.
If you think you have a urine infection (pain when passing urine, passing urine more frequently or foul-smelling urine), or if you develop a fever, it is important to contact your GP or your urologist and get treatment with antibiotics.
What follow-up will I need?
The first course of 6 x weekly treatments is called the induction course. A maintenance treatment often follows this with 3 x weekly instillations every 3, 6 and 12 months with a cystoscopy before each one. After this, you may be advised to have further “top-up” treatments every six months for up to three years.
Your urologist will organise and check cystoscopy and a clinic appointment after your course of treatment is finished.