Vasectomy
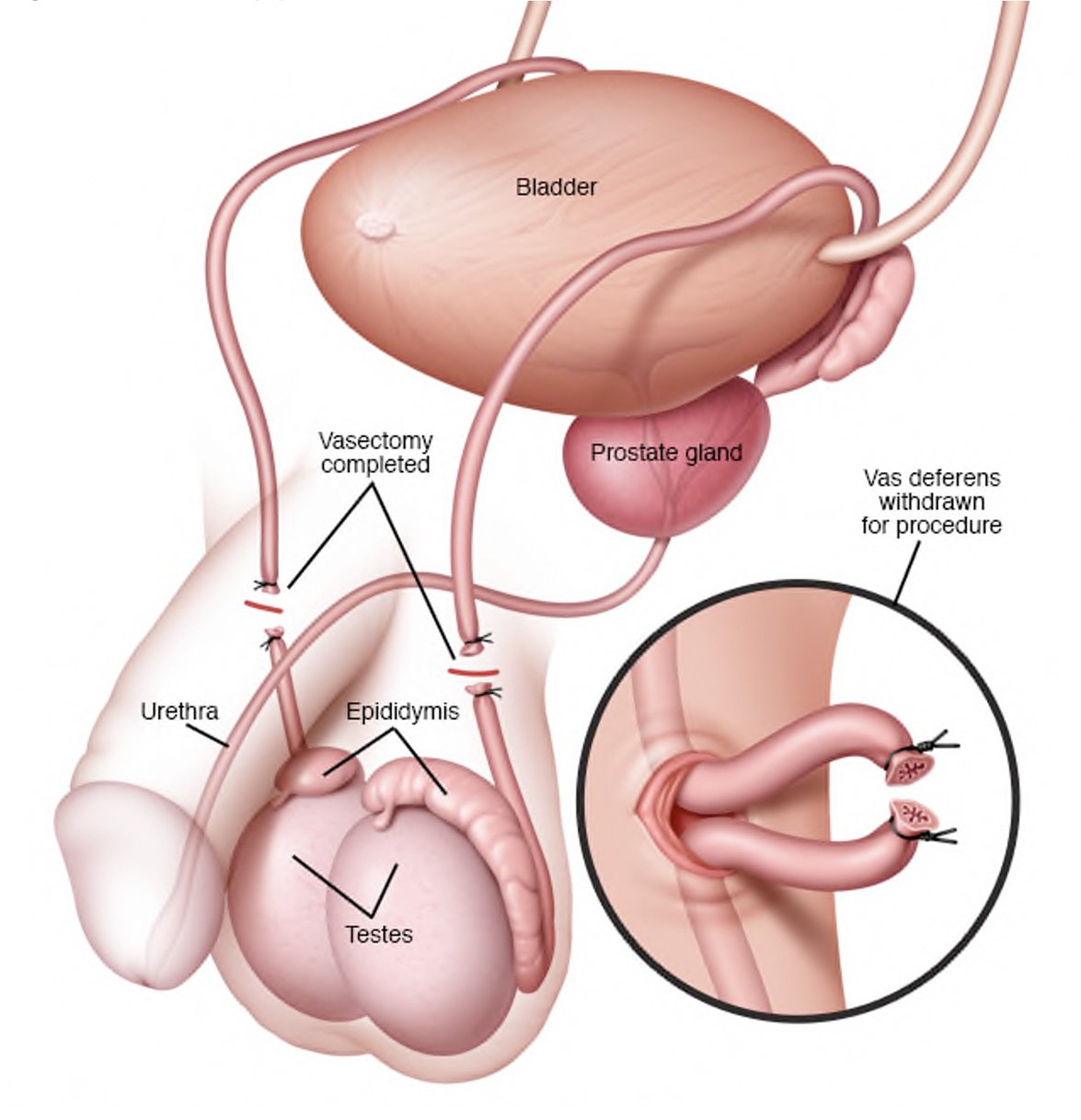
Figure 1: Vasectomy procedure.
What are the indications for a vasectomy?
The main indication is unwanted fertility. A vasectomy is a permanent contraceptive method that prevents pregnancy better than any other method of birth control, except abstinence.
What pre-operative work up is needed?
No significant work-up is needed prior to a vasectomy. Please ensure you return any admission forms given to you to be filled out back to the hospital.
What happens on the day of the procedure?
You will be given fasting instructions prior to your admission (usually for 6 hours prior to the procedure). You should bring a list of your medications with you to the hospital. After you are admitted from the admission lounge, your urologist will see you to discuss the surgery. An anaesthetist will see you to discuss the anaesthetic (usually general but can be done under local anaesthetic) before you are taken to the operation theatre.
What does the procedure involve?
A vasectomy is minor surgery to block sperm from reaching the semen that is ejaculated from the penis. Your scrotal area will be shaved and washed with an antiseptic solution. Your urologist feels for the vas under the skin of the scrotum and holds it in place with a small clamp. A tiny hole is made in the skin and stretched open so the vas deferens can be gently lifted out. It is then cut, cauterised then tied. The cut ends are paced back in the scrotum with some tissue put in between them. The small holes are closed with a dissolving suture. All these steps maximise the chance of success. The procedure is done on both sides.
Are there any risks or side‑effects of a vasectomy?
Mild pain and swelling around the surgical site lasting a few days. 40-50%
Minor infection of the incision requiring antibiotics 3-5%
A benign lump (granuloma) from sperm leaking from the cut vas 3-5%
Needing to make a bigger cut if tubes are difficult to feel under skin 2-3%
Severe bleeding or infection needing further surgery 1-2%
Chronic scrotal pain 1-2%
Early failure of procedure requiring re-do vasectomy 1/200 cases
Late rejoining of the tubes after initial success 1/2000 cases
Erections, ejacuation or orgasms are NOT affected by vasectomy
What should I expect on discharge when I get home?
You will experience some swelling and discomfort at the operative site for a couple of weeks, which should settle with time and with paracetamol and/or ibuprofen. You should wear firm supportive underwear for the first 2 weeks (avoid loose boxers). You should keep the area clean during showers and pat the area dry afterwards. The sutures are self-dissolving (takes 2 weeks) and do not need to be removed.
After 2-3 days, you can begin normal activities, driving and light duties again once you are comfortable and pain free. You should avoid strenuous activity and exercise for 2 weeks and resume these only when you are completely pain free and when your GP is happy with your progress. You should refrain from sexual intercourse for a minimum of two weeks. If you develop swelling, fevers or significant pain and redness at the site, you should contact your GP.
You MUST continue your usual method of contraception until your urologist has given you the all clear at your follow-up appointment after your two separate samples of your semen confirm no sperm.
What follow-up will I need?
Your urologist will see you in the clinic in 3 months with 2 x semen sample analysis prior. . You should ejaculate at least 20 times in this period after your vasectomy. No further follow-up is needed after this if the sperm analysis confirms no sperm in your semen.
If there are non-viable sperm in your semen, you will need follow-up semen check until this resolves. If there are viable sperm in your semen, that is classified as a failure and your vasectomy will need to be repeated. In these cases, you MUST continue your usual method of contraception until your urologist has given you the all clear at your follow-up appointment after your two separate samples of your semen confirm no sperm.