TURBT
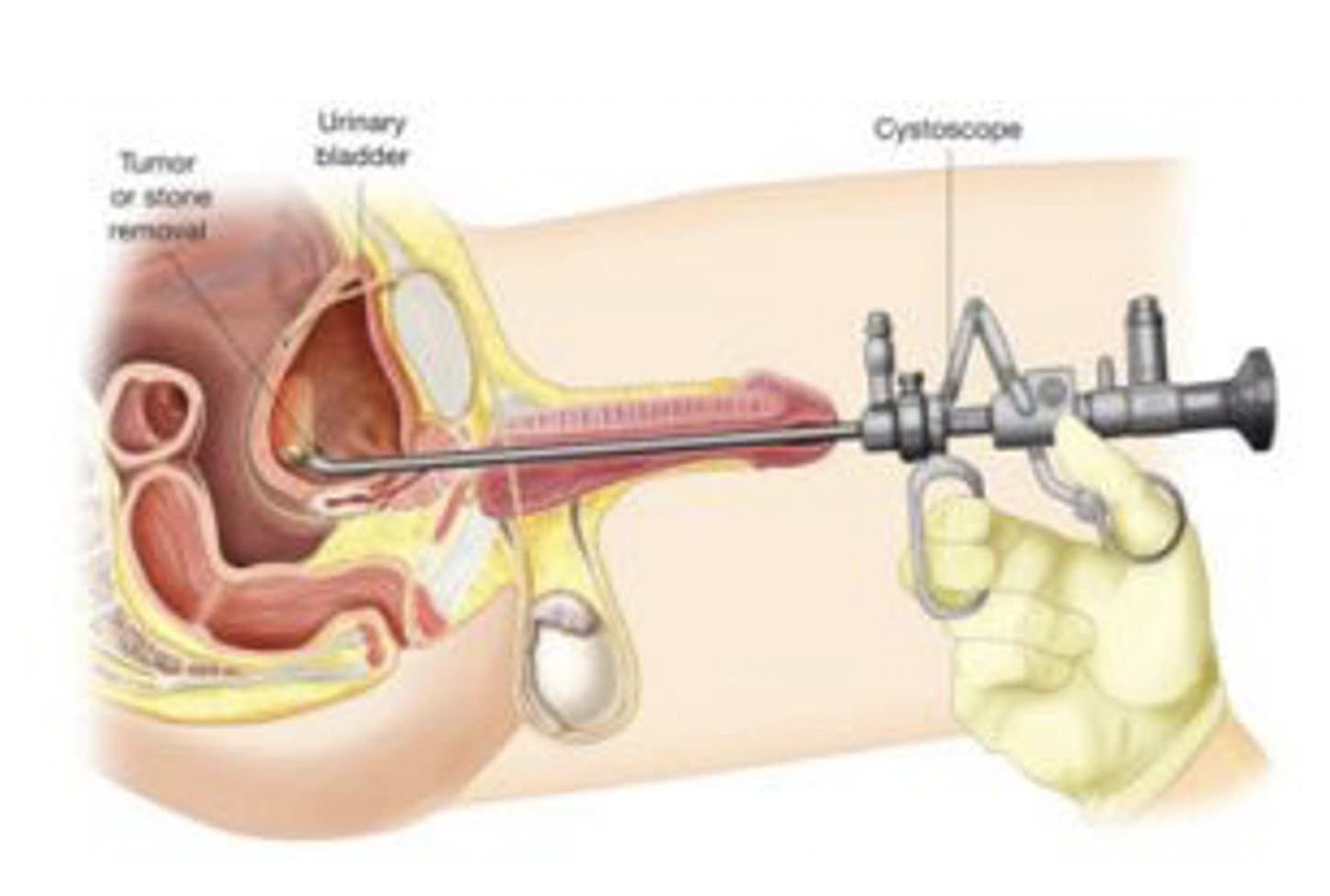
Figure 1: Transurethral resection of bladder tumour with a resectoscope.
What are the indications for Transurethral resection of bladder tumour (TURBT)?
A Transurethral resection of bladder tumour (TURBT) procedure is performed:
To confirm a diagnosis of bladder cancer
To remove tumours to reduce the risk of bleeding
To assess the aggressiveness (stage and grade) of the tumours
What pre-operative work up is needed?
Your urologist will organise any necessary urine and blood tests and imaging scans at your consultation prior to your procedure.
If you take any blood thinning medication such as aspirin, warfarin, plavix (clopidogrel) or other antocoagulants, you should discuss with your urologist if these need to be stopped before your procedure.
Please ensure you return any admission forms given to you to be filled out back to the hospital.
What happens on the day of the procedure?
You will be given fasting instructions prior to your admission (usually for 6 hours prior to the procedure). You should bring a list of your medications, any recent scans or reports with you to the hospital. After you are admitted from the admission lounge, your urologist will see you to discuss the surgery. An anaesthetist will see you to discuss the anaesthetic (either general or alternative options) before you are taken to the operation theatre.
What does the procedure involve?
Figure 2: Bladder tumour before (A) and after (B) bladder tumour resection.
TURBT involves removal of a bladder tumour (growth) from your bladder using diathermy (electrical current) or laser energy, through a telescope passed into your bladder along your urethra (waterpipe).
The procedure is done under either a general or a spinal anaesthetic. You will be given injection of antibiotics before the procedure and a telescope will be passed through your urethra (waterpipe) into the bladder to see the tumour (pictured)
Using diathermy (electric current) or laser energy, the tumour will be shaved off the bladder wall, piece by piece and any resulting bleeding points cauterised. The fragments of the tumour are removed from your bladder using suction and sent for pathology analysis.
A catheter tube will be inserted in your bladder with fluid irrigation to prevent any blood clots from forming. You may have a dose of anti-cancer drug (e.g. Mitomycin C or Epirubicin) put into your bladder immediately after the procedure; this is left in your bladder for one hour and then drained away. The procedure takes between 15 – 90 minutes depending on the size and number of tumours in your bladder. You can expect to stay in hospital overnight and occasionally longer.
Are there any risks or side-effects of a TURBT?
Mild burning on passing urine for a few days 50-100%
Blood in the urine for a few days after the procedure 30-40%
Delayed bleeding requiring further surgery to remove blood clots 2-5%
Infection of the bladder requiring antibiotic treatment 2-5%
Bladder injury requiring catheter insertion / open repair 1-2%
Urethral stricture (scar tissue formation in waterpipe) 1-2%
Damage to the ureters (tubes draining urine from kidney) 1-2%
Incomplete tumour removal 2-5%
Recurrence of tumour 20-50%
Major anaesthetic or cardiovascular problems - rare
What can I expect after discharge when I get home?
After you go home, drink plenty of fluids to flush out the blood and debris from your bladder. You may find passing urine uncomfortable at first; simple painkillers such as paracetamol or ural sachets will help with this. You may get some discharge of blood from your urethra, especially if it was necessary to “stretch” your urethra to insert the telescope.
You will pass some blood in your urine, which can last several days. If you develop fevers, severe pain or the bleeding is severe with large clots or if it stops you from passing urine, you should go to the A&E Department.
You should be able to go back to usual activities and driving after a few days when you feel comfortable and when your GP is happy with your progress.
What follow-up will I need?
Your urologist will arrange follow-up in the clinic for you in 2-3 weeks.