Hydrocele / Epididymal Cyst Repair
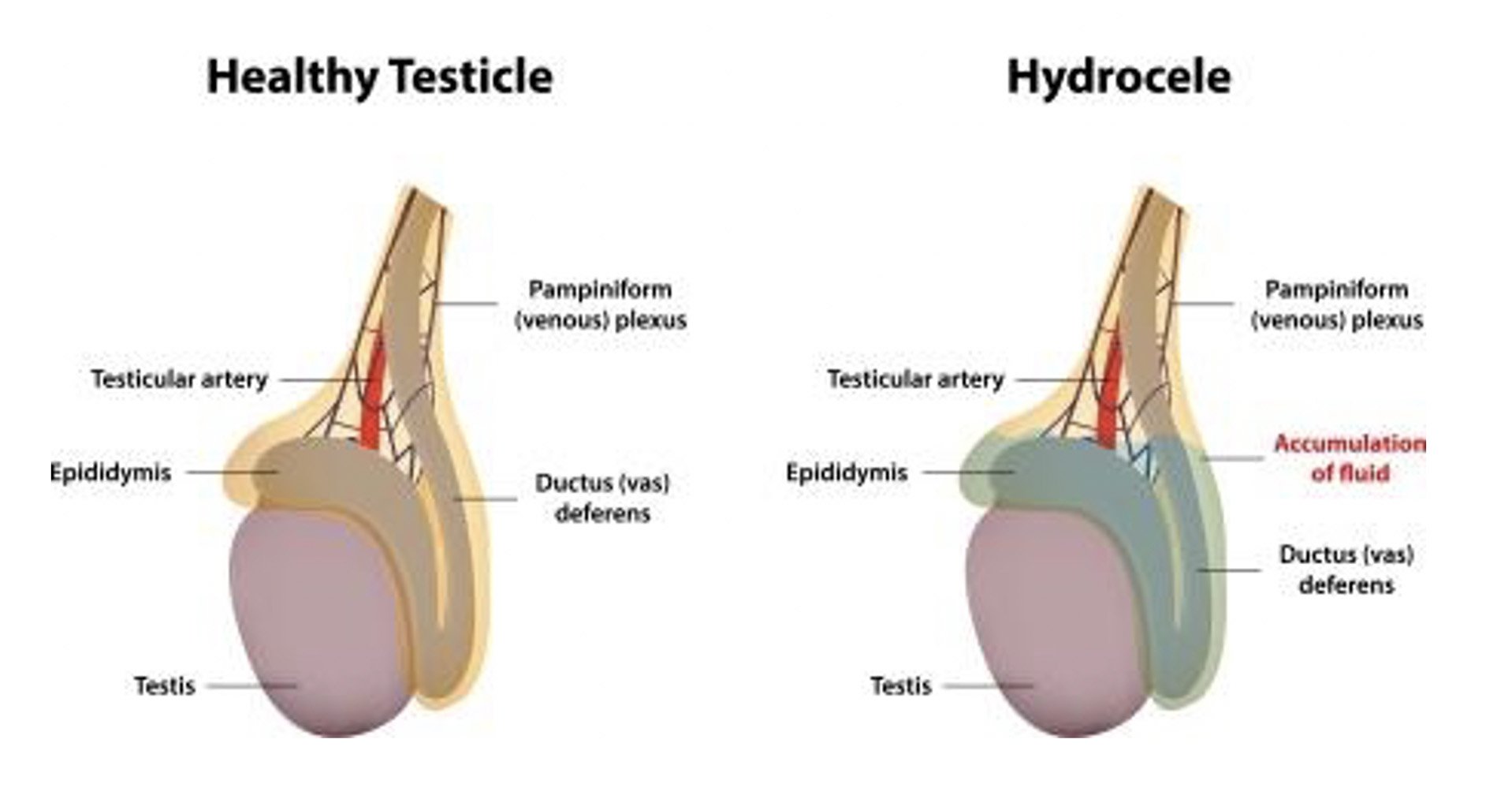
Figure 1: Hydrocele.
What are the indications for a hydrocele / epididymal cyst repair?
Hydrocele or epididymal cysts are lumps caused by a collection of fluid in the testis or epididymis, which is a long-coiled tube behind the testicles. Surgery to remove and repair a hydrocele or epididymal cyst is indicated with symptoms such as swelling, pain or heaviness.
What pre-operative work up is needed?
In most cases, no significant work-up is needed. Your urologist will organise any necessary blood tests and an ultrasound scan to confirm the diagnosis at your consultation prior to your procedure.
If you take any blood thinning medication such aspirin, warfarin, plavix (clopidogrel) and anticoagulants you should discuss with your urologist if these need to be stopped temporarily before your procedure.
Please ensure you return any admission forms given to you to be filled out back to the hospital.
Figure 2: Epididmal cyst.
What happens on the day of the procedure?
You will be given fasting instructions prior to your admission (usually for 6 hours prior to the procedure). You should bring a list of your medications with you to the hospital. After you are admitted from the admission lounge, your urologist will see you to discuss the surgery. An anaesthetist will see you to discuss the anaesthetic (either general or spinal) before you are taken to the operating theatre. You may be provided with a pair of TED stockings to wear to prevent blood clots from developing and passing into your lungs.
What does the procedure involve?
A small incision is made in the scrotum and the contents of the scrotum delivered. In case of a hydrocele (excess fluid around the testicle), the excess fluid is drained and the sac holding the fluid is inverted to prevent fluid from accumulating in the future. In case of an epididymal cyst (collection of fluid arising from the tubes that carry sperm from the testicles), the entire cyst is removed from the epididymis. Any bleeding is meticulously controlled and the incision is closed. If the amount of fluid accumulation is a lot or if there is any concern of bleeding, the surgeon may leave a drain tube to drain off any excess fluid or blood. Local anaesthetic in injected into the wound to provide pain relief. Your scrotum will be wrapped in a bandage to reduce the risk of bleeding. Simple cases may be done as a day case, however some patients may need to stay in hospital overnight and will be discharged once the drain is removed the next day.
Are there any risks or side‑effects of hydrocele / epididymal cyst repair?
Mild pain and swelling around the surgical site lasting a few days. 40-50%
Minor ooze of the wound 20-30%
Minor infection of the incision requiring antibiotics 3-5%
Need for repeat surgery due to re-accumulation of fluid 3-5%
Injury to testicle needing repair / removal 1-2%
Injury to sperm tubes resulting in impaired sperm transport 1-2%
Severe bleeding or infection needing further surgery 1-2%
What should I expect on discharge when I get home?
You will experience some swelling and discomfort at the operative site for a couple of weeks, which should settle with time and with paracetamol and/or ibuprofen. You should wear firm supportive underwear for the first 2 weeks (avoid loose boxers). Keep the bandage on for 2-3 days during which time you should avoid getting the area wet. After 3 days, you can remove the bandage. You can then keep the area clean during showers and pat the area dry afterwards. The sutures are self-dissolving (takes 2-4 weeks) and do not need to be removed.
After 5-7 days, you can begin normal activities and light duties again. You should avoid strenuous activity and driving for 2 weeks at least and resume these only when you are completely pain free and when your GP is happy with your progress. You should refrain from sexual intercourse for a minimum of two weeks.
If you develop swelling, fevers or significant pain and redness at the site, you should contact your GP.
What follow-up will I need?
Your urologist will see you in the clinic in 3-4 weeks to check everything has healed well and no further follow-up is needed after this.